Welcome to VyndaLink
You may have questions when starting a new medication. The VyndaLink team is here to support patients who have been prescribed VYNDAMAX.*
*The same VyndaLink support offerings available to patients prescribed VYNDAMAX are also available to patients prescribed VYNDAQEL ® (tafamidis meglumine).
Start Your Treatment Journey
Patient Access Coordinator (PAC)
All patients with a valid VYNDAMAX or VYNDAQEL® (tafamidis meglumine) prescription can opt-in for the support of a PAC, a Pfizer employee who can help you understand your insurance benefits, what your expected out-of-pocket costs may be, and help navigate the process to obtain your prescribed medication. Pfizer PACs are very familiar with access and reimbursement requirements and can help answer questions you may have about getting the medication prescribed by your physician.
To request PAC support, click Get Pfizer PAC support. Or, you can complete the VyndaLink enrollment form with your healthcare provider and check the box in Section 7. Please note that if you require financial assistance, the Pfizer PAC will refer you to a VyndaLink representative for further support.
Enrollment – Starting the process
Start the enrollment process today
The VyndaLink team can help you understand your insurance coverage and look for potential financial assistance options once you are enrolled.
Even if you do not enroll in VyndaLink, you will still get support. Your doctor will send your prescription directly to a specialty pharmacy, and the team there can help with insurance and reimbursement information. Expect a call from a coordinator at the specialty pharmacy.
PHARMACY LIST
Benefits Verification
VyndaLink or the specialty pharmacy will contact your insurance plan to confirm coverage for VYNDAMAX, including out-of-pocket costs, and will review the information with you by phone.

Financial Support and the co-pay savings program
Once enrolled, the VyndaLink Team may be able to help you find support to manage the cost of your medicine.
If you click on one of the buttons below, indicating what type of insurance you have, you’ll find helpful information to better understand the financial support that may be available to you.
INSURANCE
INSURANCE
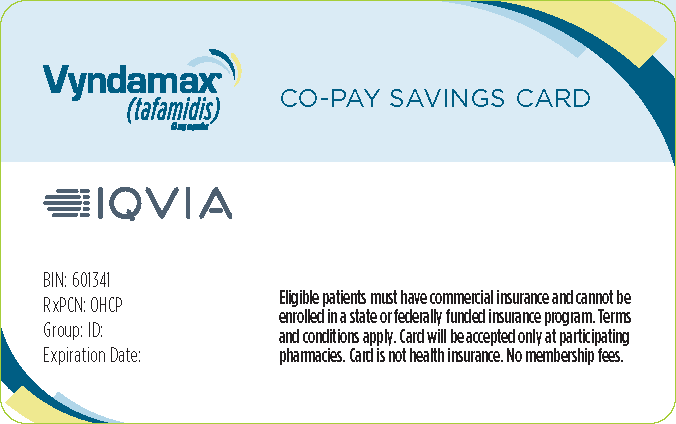
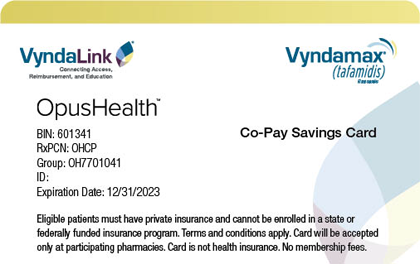
Co-Pay Savings Program for VYNDAMAX
Eligible, commercially insured patients may pay as little as $0 per month through the VYNDAMAX Co-Pay Savings Program. † Check your eligibility and download the Co-Pay Card.
Receive VYNDAMAX
A specialty pharmacy will send VYNDAMAX directly to your home. The specialty pharmacy will continue to call you to coordinate medication shipments and help with any medication issues that may arise.